April 14, 2020
Why There Aren't Enough Masks, and How to Get More
Tags:
Why There Aren't Enough Masks, and How to Get More

American hospitals are disastrously short of masks and other personal protective equipment (PPE), and demand will only increase. They estimate they will need 20x their ordinary supply over the next few months. In its current form, our supply chain cannot handle this demand shock.
In this blog post, I'll share my view of how this problem happened, and explore some ideas for how we can better serve our healthcare workers.
The current shortage of PPE is not due to a single cause. It has at least five components: insufficient inventory stockpiles, manufacturing capacity and quality control, international trade compliance, air uplift capacity, and working capital financing. And if we don't plan ahead, we'll have a sixth, involving last-mile distribution.
1. Inventory Stockpiles
The country's hospitals, medical distributors, and state and local governments don't have enough inventory for the 20x demand shock we're experiencing. The hospitals' and distributors' just-in-time inventory models were built on the assumption of normal demand. They did not account for the possibility of a pandemic.
Sadly, it seems key decision makers and regulators in the medical supply chain have not taken the lessons of “The Black Swan” by Nassim Taleb to heart. When this is all over, we will probably see new regulations about PPE inventory levels that distributors maintain as a safety stock, as well as much larger government stockpiles. Those measures might have bridged the gap, but it's too late for the current crisis, so I'll turn instead to the problems that we can address right now. Solving for the current crisis will take strong leadership, focused action, and a trusted coalition between government and the private sector.
2. Manufacturing Capacity and Quality Control
China is the only place in the world that can scale manufacturing as fast as we need right now. Our sources estimate the production capacity of Chinese PPE at 160M units per day. Of that, we believe 80M is consumed domestically and some is reserved for the Chinese national stockpile.
The US Department of Health and Human Services estimates that, throughout the pandemic, the country’s healthcare system will require 3.5 billion units of PPE. The need for quality control makes scaling manufacturing to these levels difficult. When spinning up a production line to produce PPE, a factory must ensure that the gear meets the standards required to protect workers—yet experts familiar with these specs are scarce.
Scaling QA 20x in a matter of weeks is simply impossible under existing rules. That means the US government will have to lower some standards and accept some extra degree of risk to get the numbers we need, which both the FDA and CDC have done rather aggressively.
3. Working Capital
Typically, buyers of PPE, whether hospitals or medical distributors, expect to place purchase orders and only pay for products upon delivery, or even later.
But when demand surges by 20x, vendors simply don't have the money required to scale production. Factories need money to add production lines, buy raw materials, and hire workers. They need down payments so they can move.
Buyers prefer to pay upon receipt of goods for two reasons. The first is to ensure quality: They can refuse payment if the goods they receive don't meet their standards. The second reason is they prefer to keep cash on their balance sheets, rather than paying vendors in advance.
In ordinary times, sellers will accept this. But with the entire world desperate to buy PPE, manufacturers know they can ask for a down payment and get it. Other more aggressive entities are paying down payments, so if US buyers won't, they don't get the supply.
American medical distributors, governments, and even hospital chains, by contrast, have been less willing, or less able, to adapt to the new reality of paying vendors upfront, at higher prices than they’d contracted.
At the same time, US distributors can’t pass higher prices through to hospitals in the midst of the crisis, for fear of being accused of profiteering. Foreign governments and healthcare systems have been less encumbered by this, showing a willingness to pay more and pay faster to get first in line. According to one rumor, the Italian government recently placed a $6.5B order for PPE. Another says that the UK government bought one PPE manufacturer outright.
If buyers won't pay upfront, there's another alternative for the seller: to finance the purchase order with a bank loan. But the scale of the increased demand from relatively small vendors is beyond the risk-taking capacity of most banks.
One PPE vendor that we know did $80M in revenue last year, and currently has $2B or more worth of demand for his products. They would need a 50% down payment to lock in this capacity. Even in normally functioning credit markets, this would probably be unrealistic for a business of their scale to secure. There is a lot of risk in the production process when scaling manufacturing capacity 20x. And banks have difficulty quantifying this risk, since they are not manufacturing or quality control experts. In the midst of a pandemic that has spooked lenders, getting this degree of financing is likely impossible without some form of government guarantee.
Philanthropists should also step up, lending money to organizations that have received purchase orders for PPE, but that can’t afford to buy the equipment unless they are paid upfront. Because they’ll get their money back when the pandemic subsides, this is one of the highest impact forms of philanthropy out there right now. Flexport is now working with several non-profit organizations that are actively raising impact bonds to support PPE orders, with the philanthropists getting their funds back in full when the crisis abates.
4. Freight Forwarding and Trade Compliance
The next problem facing the supply chain is scaling trade compliance to allow all these goods to clear international borders. International freight forwarders and customs brokerages have hundreds of thousands of employees doing this work in every country in the world. But,
onboarding the volume of suppliers that has emerged is a laborious process. Many of the new entrants to the market are unaware of requirements for export licensing, FDA approvals, harmonized tariff code classification, and other existing rules for clearing import and export customs.
Fortunately, the entire global logistics industry is coming together to make PPE move more efficiently. Freight forwarders have provided resources on FDA regulations so we can help customers clear shipments into the US. Quality inspection firms have ramped up testing capabilities.
The FDA has cut quite a bit of red tape, allowing certain masks labeled "not for medical use" to be used by healthcare professionals. The government has accelerated many remaining processes, making it faster than ever for importers to get their businesses and products registered. Customs and Border Protection has made it straightforward to report detained shipments of PPE for accelerated review. With these lower barriers, quality assurance becomes more important than ever—hospitals should ensure that product they’re receiving actually meets the standards advertised on the packaging.
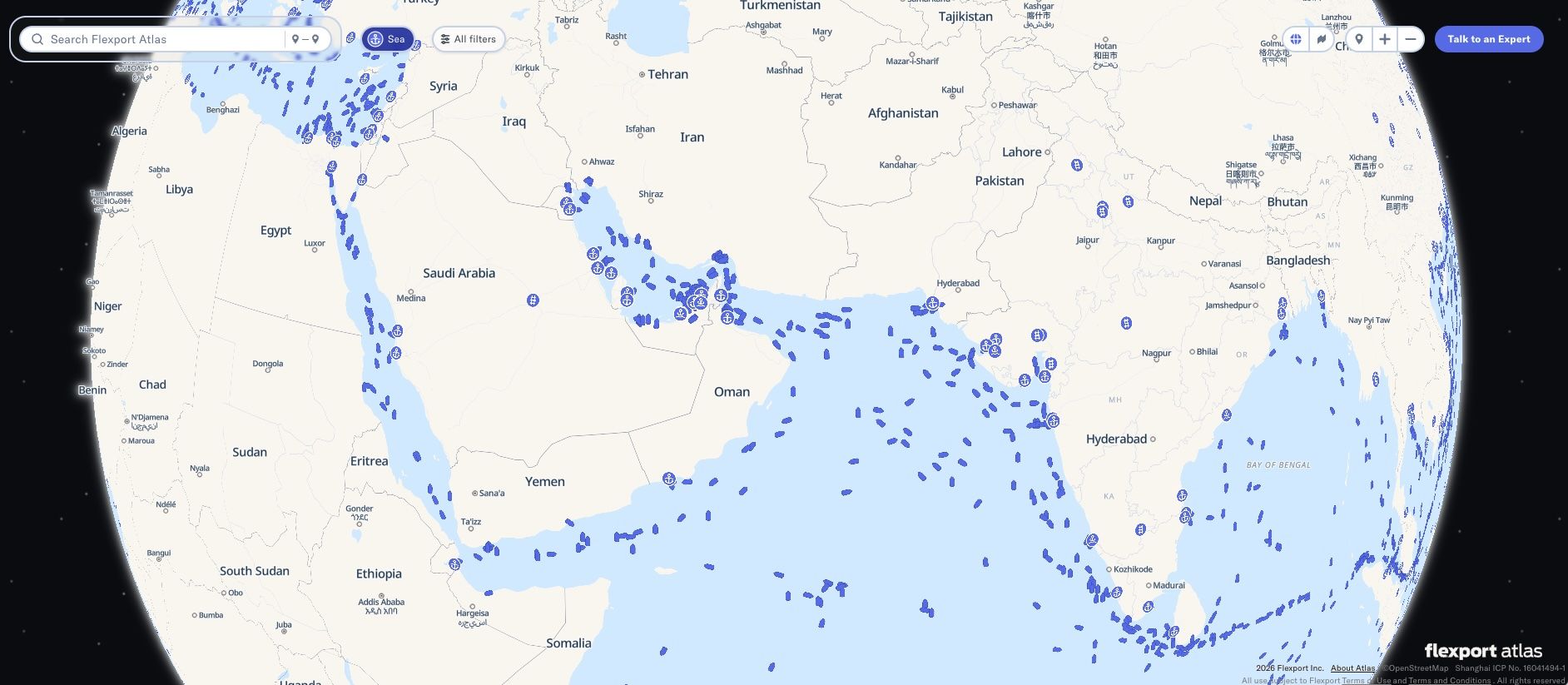
5. Air Cargo Capacity
A subset of the international freight forwarding problem is the amount of air cargo capacity available to transport it all. Half of the world's air cargo flies in the holds of passenger planes. On some lanes, like the Transatlantic, that can be as high as 80%.
With passenger fleets largely grounded due to the pandemic, there is a huge shortage of air cargo capacity required to move these goods. That shortage will grow more acute in the coming weeks as the surge of PPE starts to flow out of the manufacturing sites.
The good news is that passenger airlines around the world are stepping up to put passenger fleets back in the air as mini freighters, which will help unblock the coming logjam. At Flexport, we have signed leases with major airlines to put B789, B773 and A350 passenger planes back in the air for PPE flights. We’re doing six flights per week with two major airlines, delivering around a million units of PPE per flight. We plan to rapidly scale that program to meet the oncoming surge in demand. In addition, Flexport has purchased dedicated freighter capacity to help meet demand—500,000 kg in April, with another million set for May, just for PPE.
Military aircraft could be part of the solution, too, but the US government would have to negotiate landing rights in China—something that would be unprecedented and unexpected. If airfreight uplift capacity truly becomes the bottleneck, hopefully the two governments would be willing to work out a deal to allow this.
6. Last-Mile Distribution
Assuming we solve bottlenecks around quality control, international freight, and working capital, the final challenge will be making sure the cargo actually reaches the hospitals where it’s most needed.
The CDC needs to provide a prioritized list of hospitals for deliveries based on COVID-19 case counts, employee count, beds, and real-time PPE inventory stocks. The agency has reportedly provided this data to FEMA and HHS, but not yet to private parties looking to make deliveries of PPE. For the moment, then, we are flying blind as we attempt to route product, responding to news reports and demand signals from frontline workers and hospital administrators.
Knowing where to send the stuff is only half the battle. We also need to ensure that PPE shipments are moved quickly and efficiently from airports, where they arrive, to the correct loading docks of the hospitals. At the same time, the data should be flowing into the hospital software systems, and, ideally, back to CDC's and FEMA's data networks.
I have nightmares about unmarked cardboard boxes containing millions of units of PPE showing up on hospital loading docks, with healthcare workers forced to dig through them to find if what they need actually arrived. Even worse would be those boxes just sitting in warehouses a few miles from the hospitals because of a failure to coordinate the last-mile logistics. This sounds far-fetched, but it’s actually a well known challenge in humanitarian-relief logistics.
Up to 60% of all humanitarian aid-related product donations can’t be used immediately by the intended recipients. There were some famous cases in Puerto Rico recently, and these are not rare. It happens with the majority of all product donations for disaster relief. This is one of the reasons we started Flexport.org, to enable humanitarian organizations with powerful and easy-to-use logistics capabilities. By giving relief organizations deep discounts on freight, along with free access to our technology for SKU-level visibility, we ensure life-saving cargo reaches the end recipient, anywhere in the world.
To solve for the last mile problem, FEMA has been working directly with major medical distributors whose network includes more than 600 distribution centers across the United States. FEMA is helping to secure PPE supplies and air uplift capacity, while tapping into the distributors' existing networks to ensure the products reach the front lines as fast as possible.
Ideally, hospitals will be able to order from the medical distributors they’re used to ordering from, and have the inventory show up just like it always has.
Hospitals and related groups that order directly from overseas factories risk all manner of chaos in making sure the product actually reaches them. We saw this most recently as the Service Employees International Union fell victim to an alleged scam on an order of $39M worth of PPE they placed overseas.
We Need Leadership
Hospitals are running out of PPE and other medical supplies. The market will ramp up, but not fast enough. We need to take action to help our healthcare workers survive the next three months.
This is a solvable problem. Each of the issues above has a relatively clear short-term solution, available to policy makers and market participants right now.
We'll need support from the government to step in to buy PPE, to lease airplanes, to guarantee loans to healthcare institutions and governments, to reduce some regulations, and to run through whatever other roadblocks we encounter in the coming months.
Most importantly, we need leadership. We need someone in charge whose only job is making sure hospitals have what they need. This will mean finding PPE supplies, making sure they’re legit, buying them, and distributing them to the front lines ASAP. The White House appears to have deputized Rear Admiral John Polowczyk as the leader of FEMA’s official response to the PPE supply crisis. Given the scale of the problem and the complexity of the market failures outlined above, there’s no way for the US government to solve this on its own. But it can and must provide leadership, breaking down obstacles and coordinating the response of the private sector.
For our part, the private sector must line up to support FEMA and other government agencies in any way we’re called upon, while continuing to adapt to chaotic market conditions and working creatively to resolve these market failures.
For more about the challenges of shipping PPE, watch our recent webinar.
Please note that the information in our publications is compiled from a variety of sources based on the information we have to date. This information is provided to our community for informational purposes only, and we do not accept any liability or responsibility for reliance on the information contained herein.
About the Author